COTA’s Use of Occupational Therapy in the NICU Helps Infants Experiencing Drug Withdrawal
Katie Blahnik, a COTA in Colorado, recognized that OT could play an important role in the implementation of the Eat, Sleep, Console protocol to help infants who are experiencing drug withdrawal.

Katie Blahnik, COTA/L, NTMTC
OTA Instructor, PIMA Medical Institute
Location: Colorado
Certified in 2016
The OT Innovation
The opioid epidemic in the United States has resulted in an increased number of infants who experience in utero exposure to drugs. These infants are at greater risk for developing neonatal abstinence syndrome (NAS) as the infant withdraws from the drugs after birth. Traditionally, infants experiencing drug withdrawal are treated initially with pharmacological measures such as morphine or methadone and are automatically admitted to the neonatal intensive care unit (NICU). This may require weeks- or months-long hospital stays resulting in separation from the infant’s caregiver (parent).
Katie Blahnik, a COTA in Colorado, recognized that OT could play an important role in the implementation of the Eat, Sleep, Console protocol to help infants who are experiencing drug withdrawal. By using non-pharmacological measures as first-round treatment, especially with a heavy focus on occupational/developmental therapy techniques, Katie and her team were able to reduce hospital length of stay and costs, as well as keep the infants and their caregiver(s) together.
Through Katie’s enhanced implementation of the Eat, Sleep, Console program, OT practitioners provided therapy to Substance Exposed Newborns (SEN) six to seven times per week, rather than three to four times per week for a typical neonate in the NICU. The occupational/developmental therapy techniques and interventions utilized by the Eat, Sleep, Console care tool included sensory integration techniques such as dimmed lighting, infant massage, positioning (swaddling/sleep sacks), hearing sound (soft talking/music, limited visitors), feeding techniques as needed, vestibular input (vertical rocking, swings), swaddled baths, aromatherapy, pacifier, bonding blankets, and skin-to-skin. These techniques were incorporated into an individualized care plan for each infant and respective caregiver.
“It was very exciting to take an innovative program like the Eat, Sleep, Console method to another level by increasing the focus and addition of OT interventions. These were interventions we had previously been using for infants going through withdrawal, but adding them into this protocol allowed us to highlight the importance of OT within this population.”
Katie Blahnik, COTA/L, NTMTC
2020 NBCOT Innovation Award Winner

Producing Positive Results
Relying heavily on occupational and developmental therapy techniques allowed the infant and caregiver to room together, encouraging greater caregiver participation. It increased parental empowerment and decreased overall stress for the infant/caregiver dyad. These interventions also increased quality of life for the infant and caregiver, and reduced adverse effects caused by pharmacological measures. Caregivers reported greater satisfaction and increased confidence and empowerment in caring for their infant.
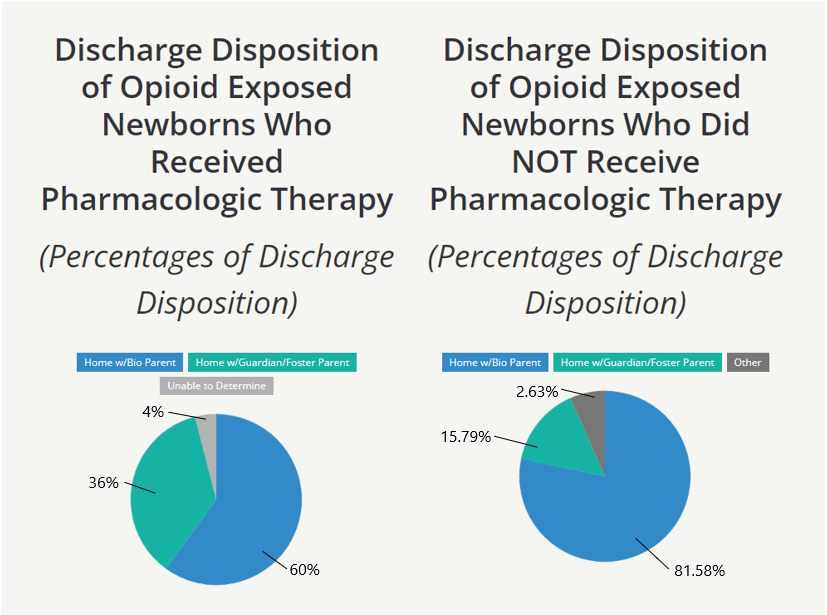
After officially implementing the program in January 2019 (it was unofficially implemented in April 2017), admissions to the NICU were drastically reduced. Over the course of the trial, the average length of stay (from April 2017 to December 2019) for infants treated with non-pharmacological measures (n=37) was almost one-third that of those treated with pharmacological measures (n=18), 4.15 days vs. 11.39 days.